Keratoconus
What is Keratoconus?
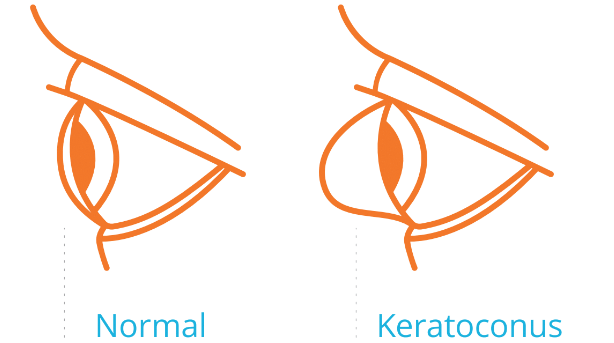
When the cornea becomes progressively weak, thin, and unstable, it gradually bulges outward into a cone shape. As the condition worsens, the cornea becomes distorted, less transparent, clouded, thinned out, and scarred.
This may take years to change, but can take place drastically for younger individuals. This leads to unusual increases in prescription, blurry and double vision even with newly updated glasses. Keratoconus affects both eyes in most cases, generally one eye worse than the other.

An example of keratoconus
Symptoms of Keratoconus
Keratoconus patients may experience some or all of the following symptoms. These symptoms become more severe as the condition progresses.
- Blurry vision
- Distorted vision
- Double vision, shadowy vision, halo or tails around light or objects
- Difficulties focusing
- Glare and light sensitivity
- Difficulties with night driving
- Drastic prescription change
- Difficulties with glasses (not clear enough, too thick, limited peripheral vision)
- Difficulties with conventional contact lenses (not clear, uncomfortable, unstable or popping out)
- Eye redness, itchiness, or discomfort
- Headache resulting from keratoconus symptoms

What it looks like to see with keratoconus
Causes of Keratoconus
The exact cause of keratoconus is not fully understood. It is believed due to be a combination of genetic, environmental and hormonal factors. Many keratoconus patients experience worsening vision over several years. Since the condition is uncommon, some patients have multiple misdiagnosis before they find out to have keratoconus. Keratoconus is usually diagnosed during the teen and early adult years. Many keratoconus patients have history of excessive eye rubbing and allergies. We treat ocular allergies so that keratoconus patients can avoid eye rubbing.
We Offer Non-Surgical Options for Keratoconus
When the keratoconus condition is mild, patients can do well with regular glasses or conventional contact lenses. As the condition gets progressively worse, glasses or conventional contact lenses cannot provide clear vision or comfort for everyday life. Specialty contact lenses designed for keratoconus offer the best vision and comfort as keratoconus progresses. There are many specialty contact lens options available for different severity of keratoconus. Sometimes the eye with more advanced condition may be best fitted with a different type of lens design compared to the eye with less advanced condition.
At Rainbow Optometry, we offer the latest contact lens technologies such as scleral lenses, corneal gas permeable lenses, Piggyback lenses, hybrid contact lenses and custom soft lenses. We are passionate to help you with these amazing, and life changing contact lenses.
What should you do when you are diagnosed to have keratoconus?
Since keratoconus is uncommon, it is generally not well understood by family members, the general public, health care providers, or even some eye care providers. Keratoconus patients may feel frustrated, discouraged, fearful, and helpless. We encourage you to stay positive, and do not give up. We are here to help you step by step to restore your vision and comfort.
These are some suggestions we would like to share with you:
- Seek eye care professionals who specialize in keratoconus
- Obtain a thorough keratoconus evaluation with a keratoconus specialist
- We highly recommend the National keratoconus Foundation Website for trusted information. The website is www.nkcf.org
- Encourage blood related relatives (siblings, cousins, children, etc.) to be tested
- Consider joining a keratoconus support group
Why should you consider us to help you?
It is our passion to provide life-changing care for keratoconus patients. We love what we do because what we do can be life changing.
- We offer a pre-appointment phone call to discuss your eye conditions.
- Our office is experienced and well trained in providing care for keratoconus patients.
- We are equipped with state-of-the-art equipment such as Pentacam for early keratoconus detection, evaluation, and progression monitoring.
- We specialize in customizing contact lenses based on the unique mapping of your cornea. We are certified as Wave contact lens fitter. Wave contact lenses offer 100% customization for your unique eye shape. These lenses can provide sharper vision, better stability, and longer comfortable wearing time.
- We comanage with opthomologists and corneal specialists for corneal cross-linking, intacs, and corneal transplants. When your eyes are recovered from the procedures, we update your glasses and contact lenses to bring forth the best results.
- Dr. Yuan is a Top Doctor 2020 & 2022 Nominee for the National Keratoconus Foundation. She is also a member of the International Keratoconus Academy and the Scleral Lens Education Society.
Medical and Surgical Treatment Options
Corneal Cross Linking (CXL)
Corneal Cross Linking is a minimally invasive procedure for the treatment of progressive keratoconus. The goal of the procedure is to slow down or prevent further progression of the condition. It is not a refractive surgery. New glasses and/or contact lenses need to be updated after CXL.
Intacs
Intacs are clear, arc-shaped implants that are surgically placed on the cornea. Intacs aim to create a more symmetrical and flattened cornea, potentially leading to reduction of refractive error. Intacs do not stop progression of Keratoconus. New glasses and/or contacts need to be updated after Intacs.
Corneal Transplant Surgery
Most keratoconus patients do not need to have a corneal transplant. However, when keratoconus progresses to a very advanced stage, the cornea may need to be replaced due to extreme bulging, thinning, scarring, and loss of transparency.
There are many types of corneal transplant surgeries. The full thickness corneal transplant is called penetrating keratoplasty (PK or PKP). Partial thickness corneal transplants include many options such as deep anterior lamellar keratoplasty (DALK), Descemet's stripping endothelial keratoplasty (DSEK or DSAEK) and Descemet's membrane endothelial keratoplasty (DMEK). Transplants can last decades with proper care, but individual results vary. Corneal transplant surgeries are considered generally safe, yet there are risks involved such as infections and rejections. Most patients require glasses or specialty contact lenses for clear vision following the transplant.
